National Flu Levels Remain Moderate as Virus Mix Shifts From A(H3N2) to Rising Influenza B
Seasonal influenza activity across the United States remained elevated but steady through early February 2026, according to the CDC’s FluView Surveillance Summary for Week 5 (ending February 7). After a January plateau, indicators show a mild resurgence of flu-like illness and a continuing shift in circulating viruses from near-exclusive influenza A dominance to a growing share of influenza B (Victoria lineage) detections.
Through five consecutive weekly reports, CDC data indicate that national influenza-like illness (ILI) visits and laboratory positivity have hovered around mid-season highs, while hospitalizations and mortality have slowly declined from December’s sharp peak. As of Week 5, cumulative hospitalization rates had reached 67 per 100,000 population, placing the 2025-26 season among the most intense since 2010–2011 particularly for young children and older adults.
CDC FluView Weekly U.S. Influenza Surveillance Reports, Weeks 1
CDC FluView Weekly U.S. Influenza Surveillance Reports, Weeks 2
CDC FluView Weekly U.S. Influenza Surveillance Reports, Weeks 3
CDC FluView Weekly U.S. Influenza Surveillance Reports, Weeks 4
CDC FluView Weekly U.S. Influenza Surveillance Reports, Weeks 5
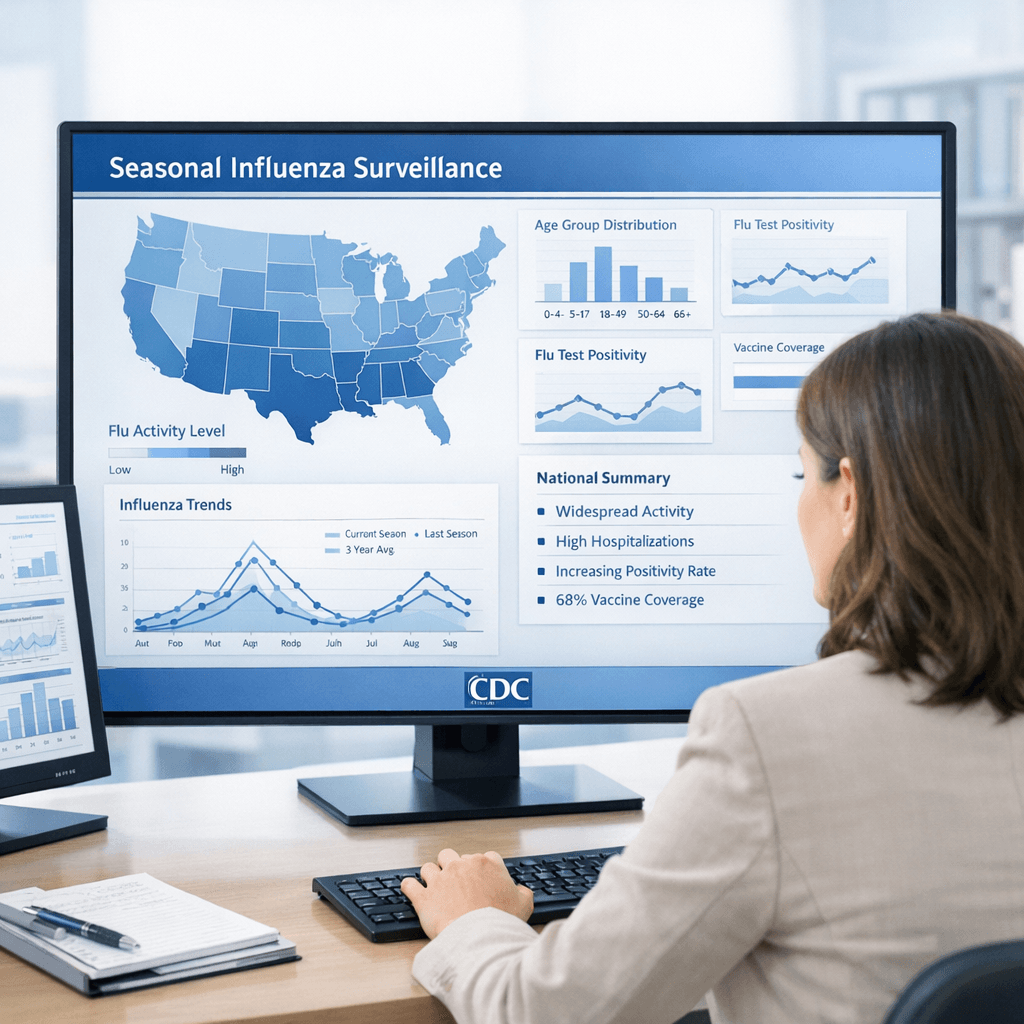
Key Nationwide Measures
Between early January and early February 2026:
- Lab positivity rose slightly from 17.7 % (Week 2) to 18.6 % (Week 5).
- Outpatient ILI visits fluctuated from 5.3 % (Week 1) → 4.4 % → 4.7 % → 4.4 % → 4.6 %, remaining consistently above the 2.8 % national baseline.
- FluSurv-NET cumulative hospitalizations climbed from 50.4 to 67 per 100,000, the second-highest at this point in the season over the past 15 years.
- Weekly admissions reported via CDC’s NHSN decreased from 27,428 (Week 1) to 14,656 (Week 5), reflecting the slow easing of severe cases.
- Mortality attributed to flu fell steadily: 2.1 % → 1.0 % of all-cause deaths.
- Pediatric deaths reached 66 for the season, with roughly 90 % of children not fully vaccinated, according to case reviews.
Influenza A(H3N2) remained overwhelmingly dominant but dropped to about 67 % of clinical detections by Week 5, while influenza B (Victoria) rose to roughly one-third of positive tests in clinical labs.
Genetic and Antigenic Profile
By early February, CDC laboratories had genetically characterized 1,766 viruses collected since late September 2025. Among the 1,126 A(H3N2) samples analyzed, 92 % belonged to subclade K, a branch closely related to current vaccine reference strains. Results indicated that 4 % of tested H3N2 samples remained antigenically well-matched, typical of this clade’s gradual evolutionary drift.
A(H1N1)pdm09 viruses showed strong stability: 97–98 % antigenic match to cell-grown A/Wisconsin/67/2022-like reference viruses. Genetic markers for antiviral resistance remained rare. Only ten A(H1N1)pdm09 isolates (≈ 0.5 %) exhibited substitutions conferring moderate to high oseltamivir resistance, while all tested viruses remained susceptible to baloxavir and zanamivir.
Influenza B (Victoria-lineage) activity doubled through January; almost all isolates belonged to genetic groups C.3.1 or C.5 subclusters variants already represented in the 2025–2026 quadrivalent vaccine composition.
Regional and Demographic Patterns
Although the overall national pattern suggested stabilization, regional differences persisted:
- Region 10 (Pacific Northwest) posted continued increases in both ILI and lab-confirmed B virus activity through Week 5.
- Mid-Atlantic and Northeast Regions (1–3) sustained gradual declines following early winter peaks.
- Southern and Plains States remained above baseline, with intermittent rebounds likely linked to local influenza B increases.
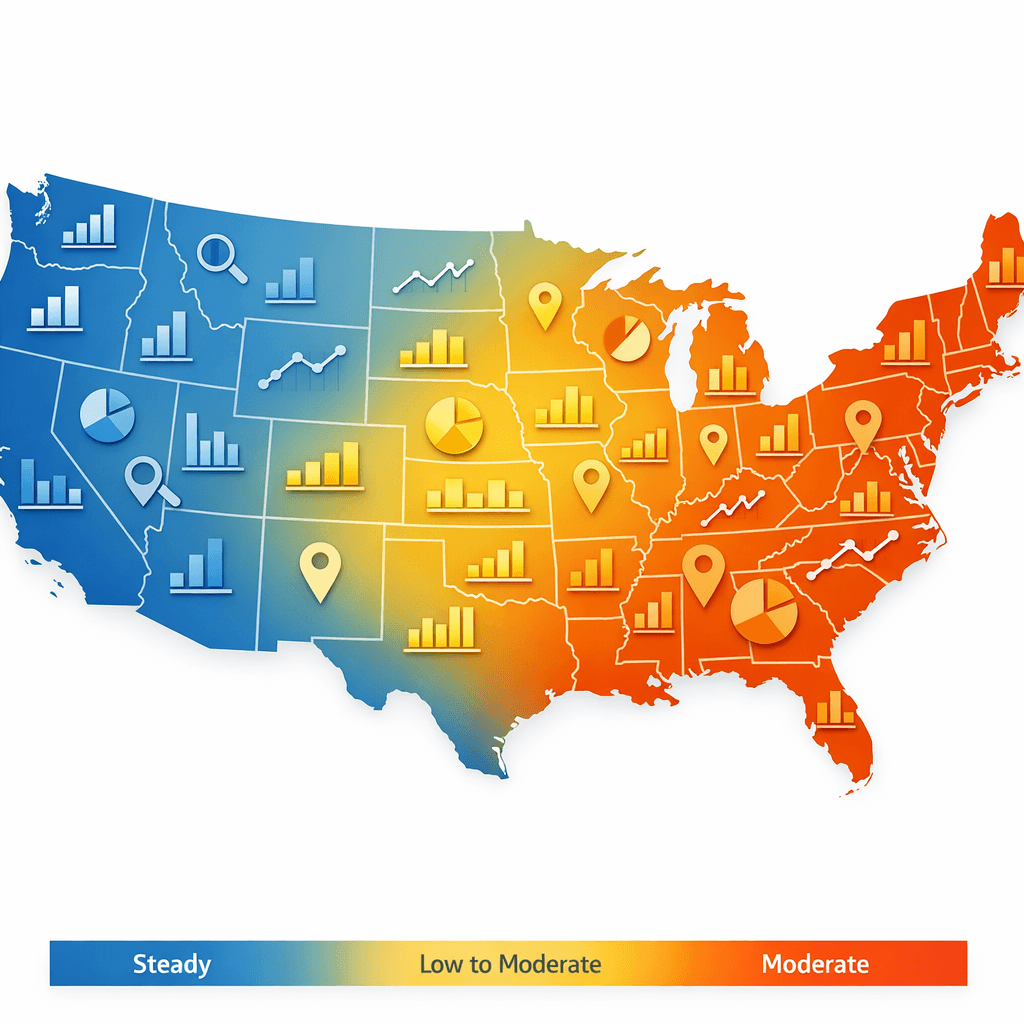
Hospitalization data reinforced well-known age disparities. Adults ≥ 65 years accounted for the highest rates (225 per 100,000), followed by children 0–4 years (68.9) and adults 50–64 years (59.5). Flu consistently produced its heaviest burden at both ends of the age spectrum.
Racial-ethnic analyses showed non-Hispanic Black Americans with the highest hospitalization rate (119.3 per 100,000), continuing a disparity long observed across respiratory-virus seasons.
Mortality and Pediatric Outcomes
CDC’s mortality tracker reported that influenza accounted for 1 % of all U.S. deaths in Week 5, a steady decline from January as severe outcomes waned.
Pediatric mortality reached 66 confirmed cases nationwide. Slightly more than half involved A(H3N2), with the remainder linked to A(H1N1)pdm09 and rising B cases. Roughly nine of ten children who died had not completed full vaccination, underscoring the enduring protective benefit of annual immunization.
Comparison With Previous Seasons
Quantitatively, the 2025–2026 season sits between the higher-intensity 2022–2023 cycle and the slightly milder 2023–2024 period. Despite localized waves, national ILI percentages peaked lower than those seen before the COVID-19 pandemic.
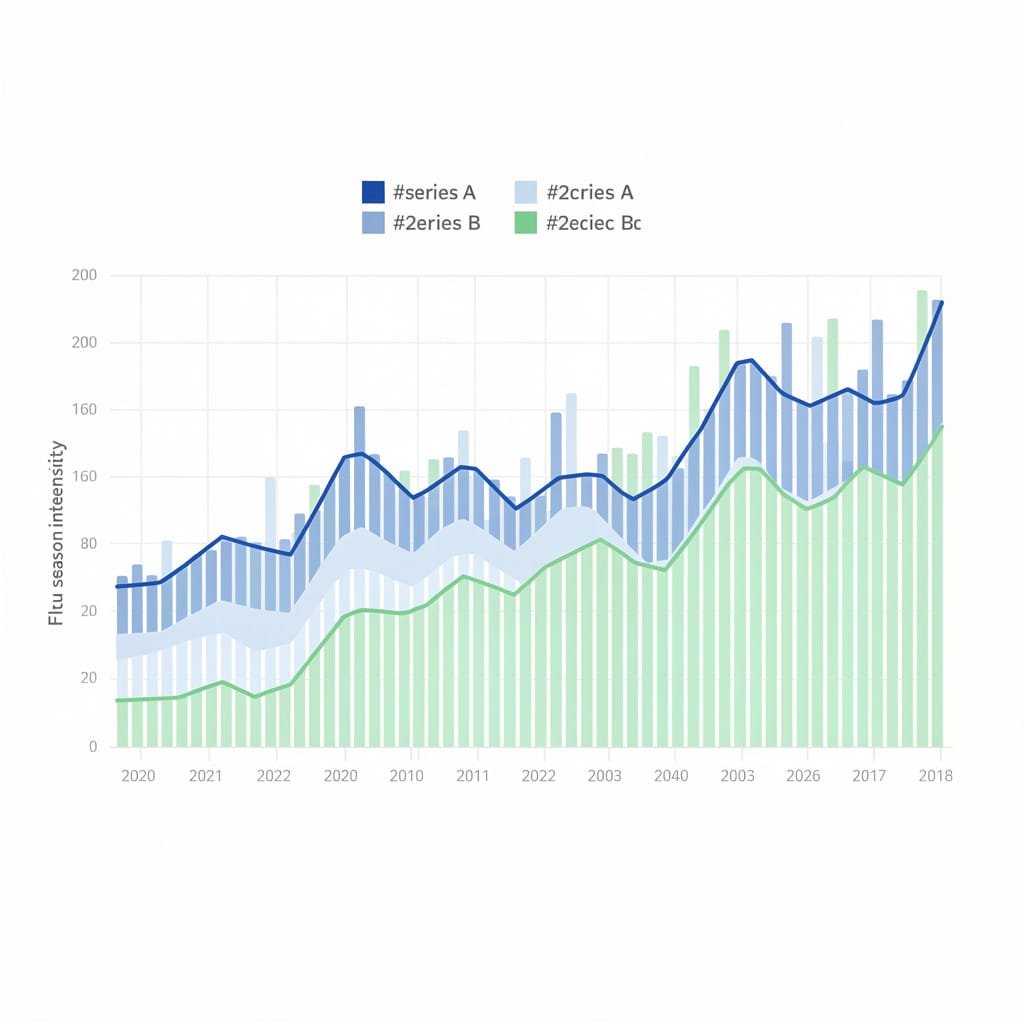
What distinguishes this season is the two-wave structure: an early December surge driven by A(H3N2), followed by a January-February plateau accompanied by a late rise in influenza B activity. CDC analysts note that this mixed-strain dynamic partly explains the flat overall positivity curve despite lower hospital strain.
Virological Stability and Treatment Sensitivity
CDC’s antiviral susceptibility testing continued to find low resistance rates (< 1%) across all neuraminidase inhibitors, comparable with historical baselines.
The agency reiterated that adamantane medications (amantadine, rimantadine) remain ineffective against currently circulating influenza A subtypes, a situation unchanged since 2009.

Nearly all antigenic results for A(H1N1)pdm09 and B/Victoria viruses aligned closely with vaccine components, suggesting that vaccine composition selected for 2025–2026 remains appropriate through mid-season.
Outpatient and Emergency Department Trends

At Week 5, 4.6 % of outpatient visits were for ILI, a modest uptick confirming persistent community transmission but below earlier-season peaks. Similar stabilized patterns were documented in the National Syndromic Surveillance System, where ED visits coded for influenza remained at 3.2 % of all visits nationally.
Age-stratified analysis revealed a recent shift: early-season activity concentrated among young children, while January-February saw relatively more visits among adults 18–49 years, likely reflecting different exposure and immunity profiles across cohorts.
Public-Health Interpretation
CDC’s in-season assessment classifies the overall severity as moderate across all ages, with high severity in children due to hospitalization rates unseen since 2010–11.
The agency continues to emphasize vaccination and early antiviral use for high-risk groups. As of Week 5, about 134 million doses of flu vaccine had been distributed nationwide. Vaccine coverage, including increased uptake of the needle-free nasal-spray (LAIV) option, remains a key driver of moderate overall impact despite active circulation of two influenza lineages.

“Flu dynamics this winter highlight the importance of timely vaccination especially for children,” said Dr. Alicia Fry, head of CDC’s Influenza Division’s Epidemiology Branch, in the Feb 13 briefing. “Even amid ongoing transmission, both injectable and intranasal vaccines continue to blunt severe outcomes.”
Global Context

The World Health Organization’s Global Influenza Update (Issue 496, February 2026) reported parallel findings: sustained but moderate activity across much of the Northern Hemisphere, with broader A(H3N2)-to-B transitions similar to those in the U.S. WHO attributed the generally muted severity to strong vaccine match and improved immune priming post-COVID-19, WHO Global Influenza Update No. 496.
Impact
For most communities, the key takeaway is continuity rather than crisis.
- Flu remains common but controlled, with hospital and mortality metrics trending downward.
- Influenza B activity is keeping the season extended but not intensifying it.
- Those vaccinated especially children and seniors continue to show lower severe-illness representation in hospitalization data.

The CDC cautions that annual patterns often include a second smaller rise in late winter, but current surveillance suggests the 2025–2026 curve is likely past its primary peak.
Scientific and Community Takeaway
The U.S. influenza landscape through early February 2026 demonstrates a system under balance: strong national surveillance, reliable vaccine matching, and moderate illness burden. Though the year’s cumulative impact rivals some pre-pandemic seasons, widespread immunization and prompt treatment have prevented the strain levels seen a decade ago.
In practical terms, the country is weathering a typical but instructive flu year: regional flare-ups, manageable hospital loads, and important reminders that consistent vaccination coverage stabilizes outcomes even in years with complex strain interplay.
This report summarizes publicly available research and should not replace professional medical consultation.

